instrument used to measure corneal thickness|how to measure corneal thickness : fabrication A pachymetry test, or corneal pachymetry test, measures the thickness of your cornea. Thickness matters for glaucoma and refractive errors, and if you’re considering eye surgery. 10 de mai. de 2019 · Download the revised edition of Midnight Club 3: Dub Edition for PlayStation 2 or Xbox. The game is a racing game with improved graphics and features.
{plog:ftitle_list}
web1 de set. de 2023 · 1. r/BrasiIeirasGostosas. 121K Members. 148 Online. 121K subscribers in the BrasiIeirasGostosas community. sub dedicado a todas gostosas do Brasil, seja ela famosa ou não! 🇧🇷.
A pachymetry test, or corneal pachymetry test, measures the thickness of your cornea. Thickness matters for glaucoma and refractive errors, and if you’re considering eye surgery.
Pachymetry can be performed by two methods, by ultrasound techniques or by optical techniques. Ultrasound Pachymetry: Ultrasound .The instrument used for this purpose is known as a pachymeter. Conventional pachymeters are devices that display the thickness of the cornea, usually in micrometres, when the ultrasonic transducer touches the cornea. Newer generations of ultrasonic pachymeters work by way of Corneal Waveform (CWF). Using this technology the user can capture an ultra-high definition echogram of the cornea, somewhat like a corneal A-scan. Pachymetry using the corneal wavefo. Pachymetry is an important part of the evaluation and management of ocular hypertension and glaucoma. Several techniques are available to reliably and reproducibly .
There are several methods used to measure corneal thickness, including ultrasound pachymetry, optical coherence tomography (OCT), and Scheimpflug imaging. . Adjusted IOP, or AIOP, describes the tonometric measure factoring in corneal thickness. Its this measure that may provide a better assessment of glaucoma risk than .Corneal pachymetry is the process of measuring the thickness of the cornea. Pachymetry is from the Greek words pachos (meaning ‘thick’) and metry (meaning ‘to measure’). The . Pachymetry is a painless, simple test that quickly measures the thickness of the cornea. A medical device called a Pachymeter is used to measure the thickness of the eye's cornea. It is used to perform corneal .
A pachymetry test is a simple, quick, painless test to measure the thickness of your cornea. With this measurement, your doctor can better understand your IOP reading, and . The pachymeteror pachometeris an instrument you dont typically find in the optometric office. This device historically has been used to measure corneal thickness for assessing corneal health related to pathologies and to evaluate corneal swelling following surgery or injury. Back when radial keratotomy was more common, refractive surgeons used . Pachymetry – A Simple Test to Determine Corneal Thickness. A pachymetry test is a simple, quick, painless test to measure the thickness of your cornea. With this measurement, your doctor can better understand your IOP reading, and develop a treatment plan that is right for your condition. The procedure takes only about a minute to measure .
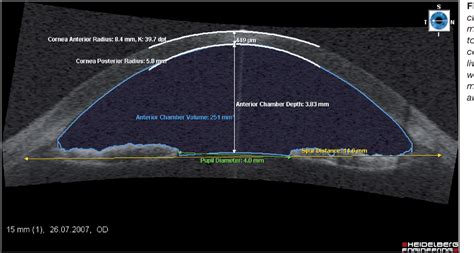
That’s where corneal topography comes in. This technology allows eye care specialists to map and measure your cornea, including its thickness and elevation changes. Corneal topography is the gold standard for mapping subtle changes in your cornea that occur suddenly or over time. Computerized corneal topography is another name for this test . To measure the corneal thickness, a special ultrasound can be used called a pachymeter. Additionally, there are instruments that use light waves to form a cross-section of the cornea called an OCT that can be measured to find the corneal thickness. How Corneal Thickness Varies. Patients with any of the following were excluded: history of previous ocular surgery, corneal disease, soft contact lens wear within one-week, dry eye, or ocular or systemic medication use that would likely affect corneal thickness. Four instruments were used for the measurement of corneal thickness: an NT-530P (Nidek Co., Ltd., Gamagori, Japan . A tangential, or instantaneous, map is very similar to an axial map. It is a slightly more accurate way of characterizing the corneal curvature but appears more "noisy" and irregular. Axial maps are less sensitive at measuring the corneal curvature and, thus, are used mainly for screening purposes (4-5).
Bland–Altman plots and intraclass correlation coefficients were used to evaluate the agreement between instruments. Results: . Derakhshan A, Daraei M. Comparison of central corneal thickness measurement using ultrasonic pachymetry, rotating scheimpflug camera, and scanning-slit topography. Am J Ophthalmol. 2010;150:780–9. doi: 10.1016/j .
The more the central corneal thickness measurement deviates from this assumption, the less accurate the measurement—thicker corneas will be overestimated and thinner corneas will be underestimated. . DO make sure your instrument is calibrated. Miscalibration of the instrument can result in systematic IOP measurement inaccuracies . Corneal thickness measurement. This test measures the thickness of your cornea, which helps your eye doctor determine your risk for glaucoma. . Then they use a tiny instrument to touch the surface of your eye and flatten the cornea, which measures the pressure. An eye pressure check doesn’t hurt, and it takes only a few minutes. But you .corneal hysteresis (a measure of corneal “stiffness”) was independently associated with glaucoma risk. Pakravan et al.30 recently reported that CCT was linked to disc size, thicker corneas being associated with smaller optic discs. Finally, Toh and associates31 in Australia recently showed that CCT is among the most highly heritable aspects of
what is a corneal thickness
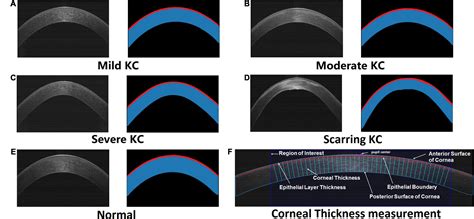
Corneal Thickness Display Map Pachymetric capabilities are only available in Scheimpflug cameras and scanning-slit topographers, since these instruments measure posterior as well as anterior surface characteristics. This display can be used to stage diseases (i.e., keratoconus), but in active contact lens wear, the primary use of this display .What is the average corneal thickness? In general the average corneal thickness measures between 540 and 560 micrometres. Cornea's over 560 micrometres are considered thick, and very thick corneas can be found in ranges above 600 micrometres.
In measuring corneal thickness, the specular microscopy technique provided values averaging 564.36 ± 32.637. The difference was 9.85, with values increased by using MS. The difference in averages between the two US and TONO investigations was 15.61 and the mean of the non-contact tonometry method 538.90 ± 35.657. Thus, we could argue that the .
Keratometer or ophthalmometer is an instrument used to measure the anterior corneal curvature and the axis and extent of astigmatism.[1] The process of these measurements is called keratometry. Hermann von Helmholtz invented the first keratometer, and it came into vogue in 1851.[2] The earlier keratometer was designed by Jesse Ramsden and Everard . Central corneal thickness (CCT) measurement has become an important test in the diagnosis and management of glaucoma. Currently, ultrasound corneal thickness measurement (pachymetry) is the most frequently used clinical technique and the gold standard to assess CCT. Newer instruments are currently available including the optical coherence . Riyam Faihan Rashid, Qasim K Farhood Department of Ophthalmology, College of Medicine, University of Babylon, Babylon, Iraq Background: The measurement of central corneal thickness (CCT) plays an .
After measurement with the Orbscan, your corneal thickness will be measured with an Ultrasonic Pachymeter. We believe in double checking everything to maximize safety. . Dr. MacRae will use the identical instrument to measure . These corneal instruments are widely used for corneal topography and not tomography assessments. These devices use a specific optical technique based on the principles of the Placido disc, named after Antonio Placido, who first described using a circular target with alternating concentric dark and light rings with a central aperture to . 9.2.9 Trans-Palpebral Tonometers . Recently instruments have been developed that measure IOP through the eyelids; examples include the Proview and the TGDc-01 [40–42].While these instruments generally are not accurate enough for regular clinical use, they may have some value in approximating IOP when ordinary tonometry is not possible, such as .
Purpose To compare central corneal thickness (CCT) measured with optical coherence tomography (OCT) using an automatic algorithm (A-OCT) vs. manual measurements (M-OCT) with respect to the gold standard ultrasound pachymetry (USP). Methods CCT measurements were performed on both eyes of 28 healthy subjects at four times of the day. A .Central Corneal Thickness (CCT) is also a significant factor in the accuracy of applanation tonometry, as the instrument was designed for an average corneal thickness of 520 microns. Patients classified as glaucoma suspects have been reported to have a higher CCT than individuals with open-angle glaucoma or healthy individuals, with 42% of . Background The aim was to compare the repeatability, reproducibility and inherent precision of ultrasound pachymetry (USP), noncontact specular microscopy (SP-2000P) and the Confoscan 4 confocal microscope (z-ring CS4) in measuring endothelial cell density (ECD), coefficient of variation of cell size (CV), and central corneal thickness (CCT) in normal eyes. . The CT-1P tonopachymetry was used to measure the corneal thickness through the principle of specular microscopy. The inclinedly emitted light from a narrow slit in the cornea is reflected by the .
Accurate measurements of the central corneal thickness (CCT) are an essential tool in management of glaucoma, since the accuracy of intraocular pressure measurements by applanation tonometry are affected by corneal thickness. 1 – 5 Accurate CCT measurements are also useful in refractive surgery because CCT is an important parameter pre- and .
ultrasound for corneal thickness
small block chevy compression test
Manufacturer Haag-Streit says that the Lenstar, which made its debut in 2009, was the first optical biometer on the market able to measure crystalline lens thickness. The Lenstar LS900 also measures AL, corneal thickness, ACD, aqueous depth, corneal curvature, radii of the flat and steep meridians, axis of the flat meridian, WTW and pupil diameter.
Central corneal thickness (CCT) is an important parameter that is routinely measured in clinical ophthalmology practice and used in the diagnosis and follow-up of ocular diseases such as glaucoma, keratoconus, and corneal ectasia. 1 However, the accurate measurement of CCT is also used to monitor corneal edema and endothelial function, to plan . The importance of precise measurement of corneal thickness, corneal curvature, and ACD has increased recently because of the development in corneal refractive surgeries and phakic intraocular lens .
small engine compression test kit
oct corneal thickness test
WEBEarn a welcome bonus of up to $250 using the Betrivers West Virginia Promo Code. .
instrument used to measure corneal thickness|how to measure corneal thickness